Signs of an Unsafe ACT Hospital System for Patients as well as Practitioners

The Chair of the ACT branch of the Royal Australian and New Zealand College of Psychiatrists Jeffrey Looi is reported to be “deeply concerned about the state of mental healthcare in the territory” and that “we are moving closer and closer to a crisis point” [i].
This follows a letter in April 2018[ii] to the Minister for Health from senior nurses and midwives at the Centenary Hospital for Women in which they raised concerns that mothers’ and babies’ lives were being put at risk by chronic overcrowding within the maternity unit; babies often readmitted due to excessive weight-loss as a direct result of being sent home early; and that women were sometimes forced to wait in pain or miss out entirely on epidurals due to the high workload of the anesthetists.
Critical media reports about Canberra’s hospital system, and in particular about patient waiting times have been appearing with increasing frequency for some years. What makes the above reports unusual is that frontline clinicians and health professionals are publicly speaking out about a “crisis” and patient safety. Clinicians do, after all, have a vested interest in assuring patients and their families that the system they are relying on in their time of illness and vulnerability is safe and deserving of their full trust. Any dismissal of health professional’s concerns as merely arising from self-interest will be simplistic and wrong. It is important to understand the state of the system and environment in which those professionals feel compelled to speak out.
In an article earlier this year[iii], we pointed out that since 2012-13, Canberra’s health system has endured funding cuts of approximately 1% per annum in real terms, when taking into account the actual population growth, ageing, changes in technology, and inflation in prices of medicines and wages. The magnitude of funding cuts is in excess of $100 million on average per annum. We also noted that, in general, rationing in service delivery systems will lead to distributional inequities unless special care is taken to ensure that the access of marginalized and disadvantaged groups is not limited. The relatively longer waiting times for Indigenous patients in the same triage category as reported by the Productivity Commission is an example of such an inequity.
There is of course an obvious link between the funding allocated to a service and the capacity of that system. Efficiency objectives, and concerns about catalytic effects on inflation in the sector can, however, either blind policy makers to the potential risks to services, or provide a simplistic justification for meeting budgetary objectives. It is relevant, therefore, to examine the effects of the funding constraints placed on Canberra’s hospital system on service capacity.
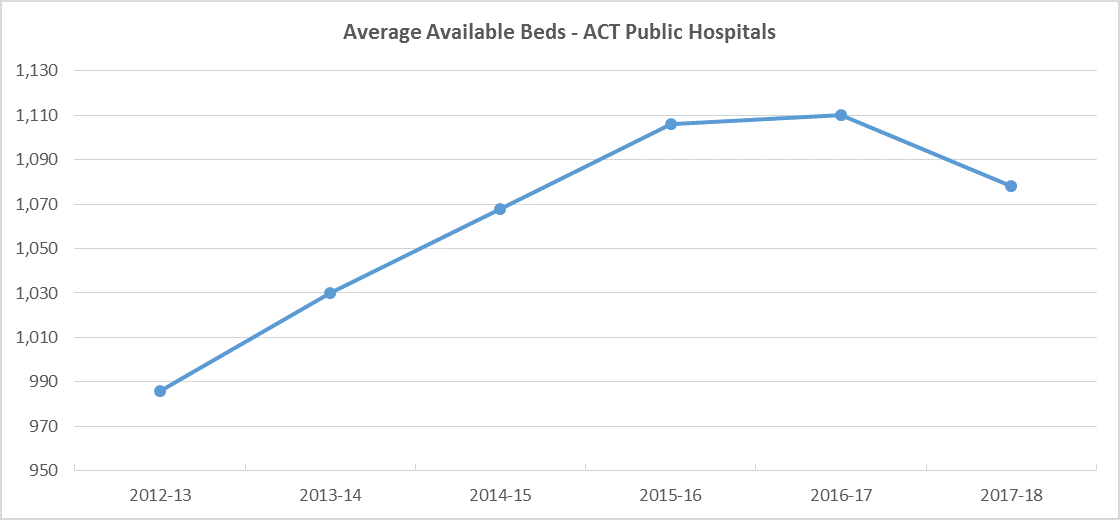
A significant measure of a hospital’s ability to deliver health care is obviously its bed capacity. The demand for beds is driven primarily by an increase in population, and increases in interventions related to ageing and improvements in technology. Technology improvements on the other hand can offset some of the increase in demand or a change in the mix of beds, for example a substitution from overnight beds to same day beds or chairs. The net effect of these changes has seen a trend increase in hospital bed capacity across Australia.
It is notable, however, that bed capacity, as reported by the Australian Institute of Health and Welfare[iv], has actually declined in Canberra’s public hospitals. In fact, over the two years from 2015-16 to 2017-18 (the last year for which AIHW data is available), bed capacity declined by 2.5% from 1,106 to 1,078 beds. By comparison, with the exception of South Australia, all other jurisdictions in Australia increased their hospital bed capacity ranging from 0.5% (New South Wales) to 6.1% (Western Australia).
In the absence of any policy measures to reduce demand, an obvious consequence of a decrease in available beds is an increase in the bed occupancy rate. It is no surprise then that in 2018-19, average bed occupancy in Canberra’s public hospitals increased to 91% against a target of 90%[v].
Prima facie, increased bed occupancy would be a sign of improved efficiency. However, it would be a mistake to draw such a conclusion. The ACT Government’s target of 90% is itself significantly higher than the accepted benchmark, which poses the risk of adverse outcomes for both patients and practitioners.
For example, a longitudinal study analysing more than 4 million patient records found that a 1% increase in bed occupancy was associated with a 0.49% rise in the discharge rate, and a 0.011% increase in the 30-day readmission rate for discharged patients[vi]. The average occupancy across the study was 90.4%.
A number of studies in hospital settings in Northern Ireland[vii], Malta[viii] and the United Kingdom[ix]have highlighted evidence of adverse patient outcomes as bed occupancy rate increases beyond 85%. In particular, the spread of Methicillin-Resistant Staphylococcus Aureus (MRSA) in hospitals has been shown to correlate with bed-occupancy rates.
For patients presenting to emergency departments, studies in England, Canada, Australia and the United States conclude that high bed occupancy results in access block[x], increased length of stay[xi], and delayed discharge and admission to ward progressively above bed occupancy rates of 80%[xii]. Emergency department overcrowding due to access block has been found to result in higher in‑hospital patient mortality[xiii].
High bed occupancy rates have not only been shown to compromise timely treatment and patient outcomes, a significant association has also been noted between high hospital bed occupancy rates and the initiation of antidepressant therapy among nursing and medical staff[xiv]. This is not surprising given that an overcrowded hospital with patients stuck at various points will become increasingly more stressful for health professionals seeking to deliver care.
So, what is an appropriate level of bed occupancy beyond which hospitals are less efficient and safe? While the precise figure may vary from hospital to hospital depending upon its patient mix and their arrival times, the general consensus based on the available evidence is that bed occupancy rates above 85% impact negatively on the safe and efficient operation of a hospital[xv].
It is notable that the bed occupancy rate in ACT public hospitals in 2009-10 was 86%, which progressively increased to 93% in 2012-13, against a target of 85% for those years. In 2013-14, the target was changed with the following note in the Annual Report[xvi]:
“The long-term target is to maintain bed occupancy levels for best patient outcomes and to achieve maximum efficiency. However, with increasing pressure on ACT public hospitals each year, the ACT target for this indicator in 2013–14 was revised to 90 per cent. This recognises a more realistic target in the transition period while the necessary infrastructure and process improvements take effect, which will allow ACT public hospitals to achieve the 85 per cent in coming years.”
Five years on, the target remains at 90%, and even the aspiration of achieving 85% bed occupancy appears to have been abandoned.
Worryingly, due to its failure to invest in hospital capacity, the Government has persisted with the “realistic” approach of simply changing the target, albeit, making the hospital system less safe for patients as well as practitioners. On the basis of published research, it is reasonable to expect an increased likelihood of preventable adverse events for both patients and staff in Canberra’s public hospitals.
[i]See https://www.canberratimes.com.au/story/6473079/acts-mental-health-system-on-brink-of-crisis-psychiatrists/?cs=14229
[ii] See report in The Canberra Times https://www.canberratimes.com.au/story/6018569/maternity-staff-at-breaking-point-patient-safety-cant-be-guaranteed/.
[iii] https://www.canberratimes.com.au/national/act/the-act-government-is-shrinking-health-spending-year-on-year-20190319-p515fd.html
[iv] Australian Institute of Health and Welfare (2019); Hospital Resources 2017–18: Australian Hospital Statistics: https://www.aihw.gov.au/reports/hospitals/hospital-resources-2017-18-ahs/rep2ort-editions.
[v] ACT Government (2019); Annual Reports, 2018-19: Canberra Health Services, Page 27.
[vi] Friebel R, Fisher R, Deeny SR, Gardner T, Molloy A and Steventon A. The implications of high bed occupancy rates on readmission rates in England: A longitudinal study. Health Policy 2019, 123(8): 765-772.
[vii] Cunningham JB, Kernohan WG, and Sowney R. Bed occupancy and turnover interval as determinant factors in MRSA infections in acute settings in Northern Ireland: 1 April 2001 to 31 March 2003. J Hosp. Infect. 2005; 61: 189-193.
[viii] Borg MA, Suda D, and Scicluna E. Time-series analysis of the impact of bed occupancy rates on the incidence of methicillin-resistant Staphylococcus aureus infection in overcrowded general wards. Infect Control Hosp Epidemiol 2008; 29: 496-502.
[ix] Kibbler CC, Quick A, and O’Neill AM. The effect of increased bed numbers on MRSA transmission in acute medical wards. J Hosp Infect 1998; 39: 213-219.
[x] Cooke MW, Wilson S, Halsall J, Roalfe A. Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J 2004; 21: 575-576. 14 Forster AJ, Stiell I, Wells G, et al. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med 2003; 10: 127-133.
[xi] Richardson DB. The access-block effect: relationship between delay to reaching an inpatient bed and inpatient length of stay. Med J Aust 2002; 177: 492-495.
[xii] Hillier DF, Parry GJ, Shannon MW, Stack AM. The effect of hospital bed occupancy on throughput in the pediatric emergency department. Ann Emerg Med 2009; 53: 767-776.
[xiii] Richardson D. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006; 184: 213-216.
[xiv] Virtanen M, Pentti J, Vahtera J, et al. Overcrowding in hospital wards as a predictor of antidepressant treatment among hospital staff. Am J Psychiatry 2008; 165: 1482-1486.
[xv] Keegan AD. Hospital bed occupancy: more than queuing for a bed. Med J Aust 2010; 193: 291-293, and references therein.
[xvi] ACT Government (2014); Annual Report, 2013-14: ACT Health Directorate, Page 25.
Image: By Dfadden - Own work, CC BY-SA 3.0, /eb25a55437b8d842543856b55a6080f7/w/index.php?curid=25574500

